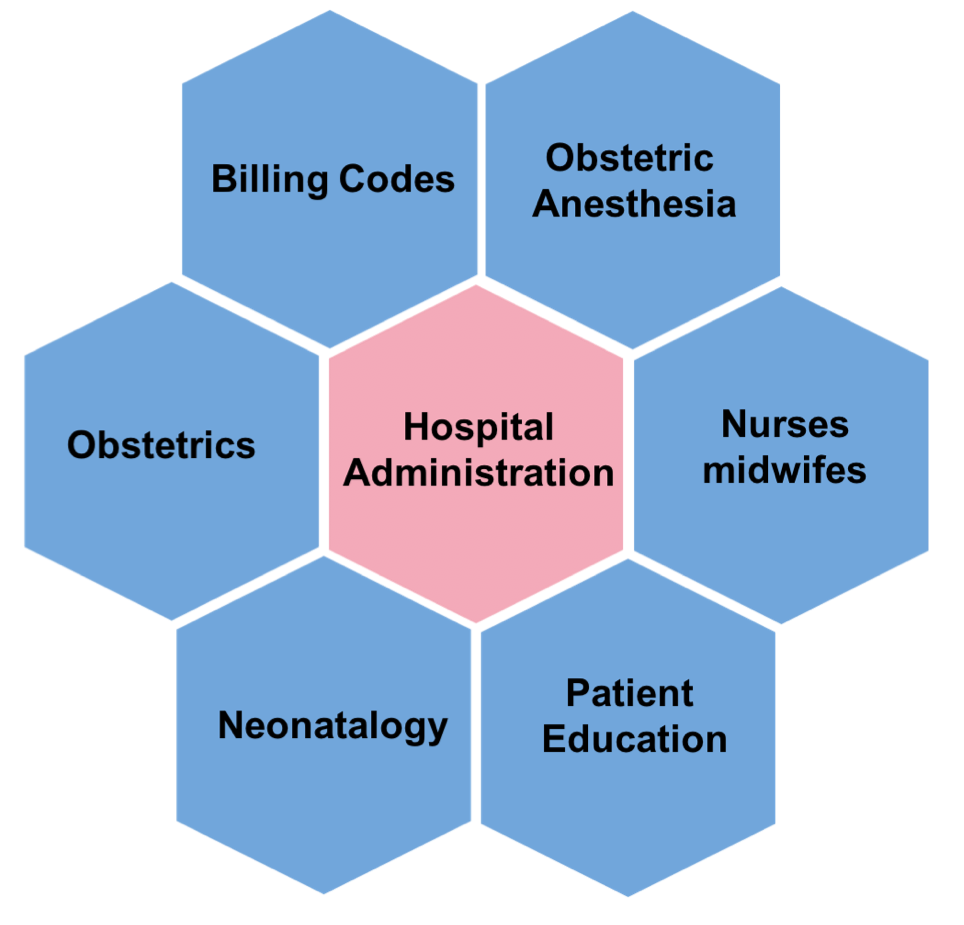
Patient education:
The number one concern surrounding labor analgesia (labor pain relief) in both Chinese-speaking and non-Chinese mothers alike is the safety of the baby. Although only a small dosage of narcotics (or pain relievers) enter the bloodstream when the epidural is administered, many mothers in China remain concerned about the effect of these narcotics on their babies and the possibility of narcotic addiction. Additionally, many believe the financial cost of the procedure is unnecessary and that the added labor pain will strengthen the pair-bond between mother and child.
To further complicate the matter, many medical procedures in China, including labor analgesia, must be consented to by both the biological mother and father. Because of this situation, it is imperative that the patient’s family be completely informed about the nature of the medical procedures.
Oftentimes, medical providers misinform patients about neuraxial labor analgesia because of the limited amount of experience medical professionals in China have with this area of medicine. The standard of care for neuraxial labor analgesia also varies greatly from region to region, which results in mixed clinical outcomes and patient satisfaction, again reinforcing the misconceptions concerning the safety of this procedure to both providers and patients.
Some common questions and concerns are:
Is it safe for my baby?
What can I do if my husband (or other family members) disagree about labor analgesia?
I have an epidural, why am I still suffering from labor pain?
If I am gestational diabetic, can I still have an epidural?
My obstetrician told me the best way to delivery my baby is through caesarean section.
Anesthesia:
Little anesthetic manpower is available. Anesthesiologists have not received much support for neuraxial labor analgesia by hospital administrators, largely due to poor financial reimbursement. Another challenge has been to rectify the perception that neuraxial labor analgesia is merely a technical procedure: the placement of an epidural catheter. The medical management of a patient’s neuraxial labor analgesic has been left out of the equation. This has also led to an underestimation in manpower requirements. Currently, few obstetric anesthesia services are able to provide full coverage during the day on weekdays.
Another issue has been the language barrier. The vast majority of obstetric anesthesia publications are written in English. This has limited the availability of new literature to the majority of Chinese obstetric anesthesiologists. This has contributed to practices that are not evidence-based. For example, in China, most neuraxial labor analgesia is limited to the active phase of the first stage of labor. No pain relief is provided for the early first stage or the second stage of labor because it is believed to be unsafe.
Obstetrics:
The majority of Chinese obstetricians do not have experience with neuraxial labor analgesia because they have many concerns about its safety, impact on daily obstetric practice, and possible complications. Some common arguments include:
It does not work.
It will prolong the second stage of labor.
It causes fetal distress.
It causes lower back pain.
It increases postpartum hemorrhage risk.
It should not be used in high-risk obstetric patients.
It has increased our cesarean delivery rate.
We just cannot provide labor analgesia during the second stage of labor.
Neonatology
There are lots of misconceptions about neuraxial labor analgesia. They believe that those babies have more chance of meconium staining, lower Apgar score, fever and antibiotics use.
Nurses/midwifes:
Midwives in China have different clinical duties than midwives in the United States. Like midwives in the US, Chinese midwives are also responsible for intrapartum obstetric care; however, unlike US midwives, they must also perform the clinical duties of the labor and delivery nurse. Because of this, the limited number of midwives leads to decreased attention to the influx of new patients and significantly decreased standard of care for each patient individually. In addition, learning and implementing new knowledge and skills are universally challenging.
For these midwives, neuraxial labor analgesia imposes seemingly unnecessary additional work. Laboring women arrive earlier to initiate the the peripheral IV, and midwives must prepare for the patients, monitor them after the administration of neuraxial labor analgesia, and communicate with anesthesiologists. These services increases the demand for midwives and labor & delivery nurses, which hospitals often cannot accommodate.
Because of the critical role midwives play in Chinese labor & delivery rooms, collaboration with them is crucial to success in neuraxial labor analgesia. As of now, midwives in China may be able to perform clinical interventions, such as an episiotomy, and their scope of practice has recently increased to include caring for high-risk patients. They have the potential to play a unique role in educating their patients about neuraxial labor analgesia.
Billing codes:
Chinese medical bills are based on a set of medical billing codes. Without a billing code, patients cannot be billed for the medical service, even if patients were willing to pay out of their own pockets. One major challenge has been defining appropriate billing codes within hospitals to better reflect the medical services that are provided by obstetric anesthesiologists in order to improve the availability of obstetric anesthesia services.
Hospital administration:
Hospital administrators have had minimal experience with obstetric anesthesia. This is mainly due to the fact that obstetric anesthesia has not been a revenue generator for Chinese hospitals. As previously mentioned, one huge challenge has been to define appropriate billing codes for obstetric anesthesia services. Without this, obstetric anesthesia services do not generate adequate revenue for the hospital, and without an adequate revenue stream, it becomes difficult to request additional manpower and the purchase of new equipment and supplies. This only serves to reduce patient access to obstetric anesthesia care.
| |
|
|
|
|
|
|
|